My BFF Has Genital Herpes

Her life-changing news altered my thinking about sexual health.
On the morning of my 26th birthday I went to work thinking about seeing my friends at the bar later. My best friend Abby* had just returned from visiting another friend out of state and I couldn’t wait to see her and hear what they had gotten up to together. I knew I wouldn’t be able to focus on my work for the rest of the day. That ended up being true, but for a reason I never expected.
At 10am that Wednesday my cellphone started buzzing. It was an odd time for Abby to call so I picked up right away, knowing something had to be wrong. She was crying. I begged her to tell me what was going on. She hesitated before answering, but eventually got the words out. She had just found out she had genital herpes.
My first instinct was to comfort her. I repeated, “It will be okay.” But would it be? I wasn’t sure. Abby was not the first of my friends to confide in me about an STI. Two years earlier, when a close guy friend told me about his uncomfortable symptoms and subsequent gonorrhea diagnosis, the mood was somber and reflective, but not nearly as heavy. A gonorrhea infection can be cured with a round of antibiotics.
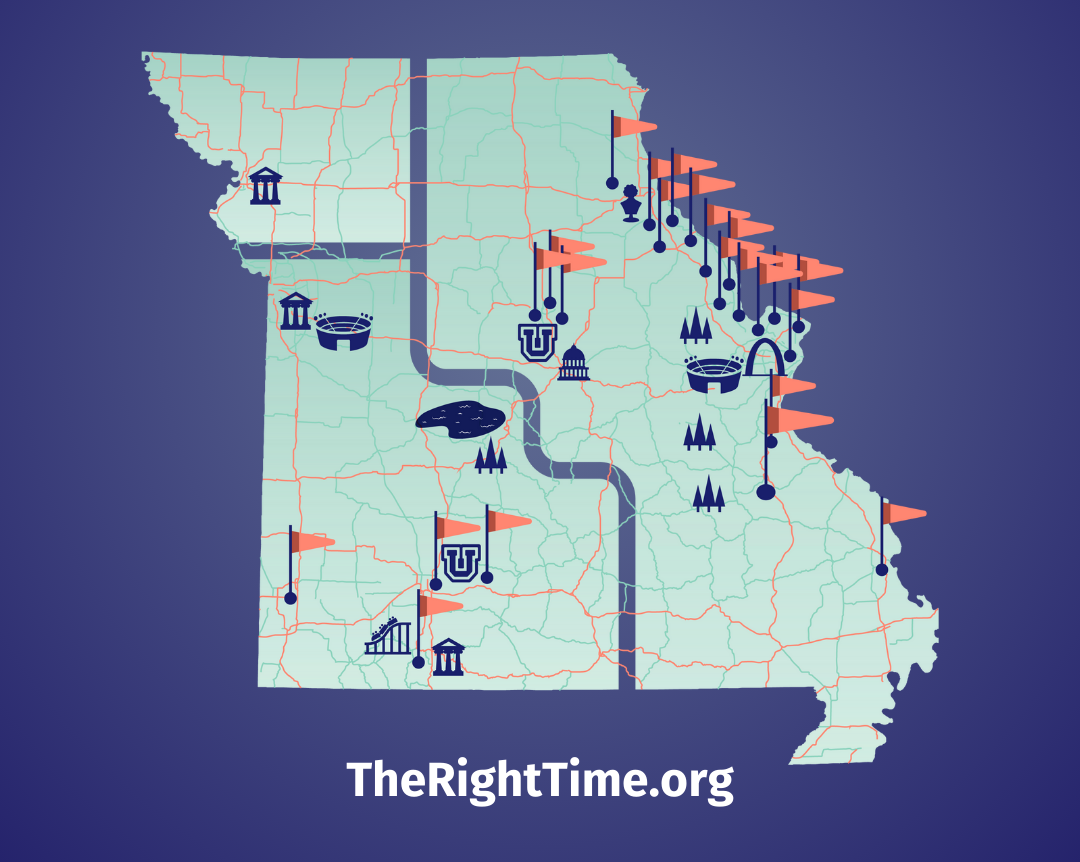
By the end of the phone call I had soothed her a bit and learned a really unfortunate detail about the situation. She believed she had contracted the virus from the person she was visiting, our mutual friend. Still at work and unsure of what to do next, I turned to Google (if you think you might have genital herpes, or another STI, make an appointment with a provider at your nearest The Right Time health center).
Getting informed
Like many people, my knowledge of herpes before Abby called that day was based on a little bit of health class and a lot of social stigma. I “knew” that it was with you for life and would impede the chances of forming meaningful romantic relationships or having just-for-the-fun-of-it, no-strings-attached sex. I “knew” that it would be a painful reminder for years of a single encounter that she probably could have avoided or prevented.
Questioning my own understanding of herpes, I read as much as I could. A lot of what I found was actually comforting. It is more difficult to transfer the herpes virus from a female to a male than the reverse, reducing Abby’s risk of transmitting the virus to a partner. Also, she had tested positive for HSV-1, which is usually associated with oral herpes. HSV-1 typically produces fewer outbreaks over time than HSV-2, another strain of the herpes virus. Those are things she could share with someone she plans to be intimate with.
By the next time we spoke, Abby had also found a lot of information online and had another conversation with her doctor. Unfortunately, some of the facts and statistics we had each found were conflicting. The inconsistencies made Abby worry. She didn’t know what to expect.
Abby frequently wondered out loud about whether she had contracted herpes from our friend or another partner. There were lots of charts online and in magazines with average timeframes between infection and a first outbreak, but herpes can lie dormant for so long that none of them could provide a clear answer.
The mystery plagued me as well, but I knew no answer would reverse what had occurred. Knowing that it would be close to impossible to figure out who she’d gotten it from, I helped her redirect her energy into how she could manage the virus.
Prescription medications could help reduce the frequency and duration of Abby’s outbreaks, but there was no way to tell how often she would suffer from flare-ups. Although medication could help with the pain and discomfort of herpes, it wouldn’t save Abby from having to talk to future partners about it.
Herpes can be transmitted whether or not a person is experiencing an outbreak. For all of my research, at the time I still thought Abby would only be able to date people who also had genital herpes. Though I had cut through the stigma on my fact-finding mission, I imagined that her potential partners might not be very understanding or informed.
Big lessons
I didn’t always feel like I was being the best friend I could be to Abby. At times, I caught myself being ruthlessly judgmental. Maybe this wouldn’t be happening if she had agonized over using protection as much as she did trying to determine who gave her herpes. I was, and sometimes still am, guilt-ridden over those moments even though I didn’t vocalize any of it.
When Abby told me another friend had become overly cautious about sharing personal items, her hurt was palpable. I realized what a responsibility I had to her and to our friendship to make her feel just as comfortable and loved as she had before she contracted herpes.
Whether or not she could have prevented it, my job as a friend is to be supportive and constructive, not to reprimand her or make her feel guilty.
Abby’s diagnosis changed my whole perspective on sexual health. I had always felt that having open conversations with partners about testing and STI status, along with scrupulous use of barrier methods, would virtually eliminate my chances of ever contracting anything. Turns out that prevention can be complicated—especially when it comes to herpes.
I knew on some level that oral herpes could be transmitted via non-sexual contact, and that genital herpes could find its way around condoms, but those risks felt negligibly low. It’s possible that Abby contracted the virus via oral sex. I don’t think I’ve ever seen a dental dam in real life or heard of a friend using one. I’ve put myself at the same amount of risk that Abby had. And for all of my asking partners about their status, “Do you have oral herpes?” or, “Have you ever had a cold sore?” were questions I’d never thought to ask.
One year later, everything feels different. So many other things have happened in both of our lives that make herpes seem, while still serious, a lesser concern than it did when Abby first called on my birthday. Abby is in a great relationship with someone who is STI-free and totally accepting of the fact that she isn’t.
Contracting an STI, even one for which there is no cure, didn’t change my friend or ruin her chances for a fulfilling life. Though it seemed impossible that the person I knew could find herself in this situation, that was only because of my own ignorance. Now, we’re both a little bit smarter about sexual health, and our friendship is stronger than ever.
The Dos and Don’ts of Supporting a Friend with Herpes
- Do your research. The more you educate yourself the more effective you can be in supporting your friend.
- Don’t start treating your friend differently. She’s the same person you’ve always loved and cared about.
- Don’t jump to conclusions. Herpes may be easier to transmit than you think and contracting it does not mean your friend was being especially careless.
- Do make improvements to your own sexual health practices. Now that you know more about herpes, you can better protect yourself.
*Names changed
Updated January 2020
Related Content


Article
What Does “Dual Protection” Birth Control Mean?It usually means using a condom along with another birth control method.

Article
January is Cervical Cancer Awareness Month: What to Know About HPV and ScreeningA positive HPV test can feel scary, but healthcare providers at your nearest The Right Time clinic can help.

Article
Own Your Well-Being in 2026 with These 3 Sexual Health ResolutionsFirst: prioritize preventative sexual and reproductive health care.