January is Cervical Cancer Awareness Month: What to Know About HPV and Screening

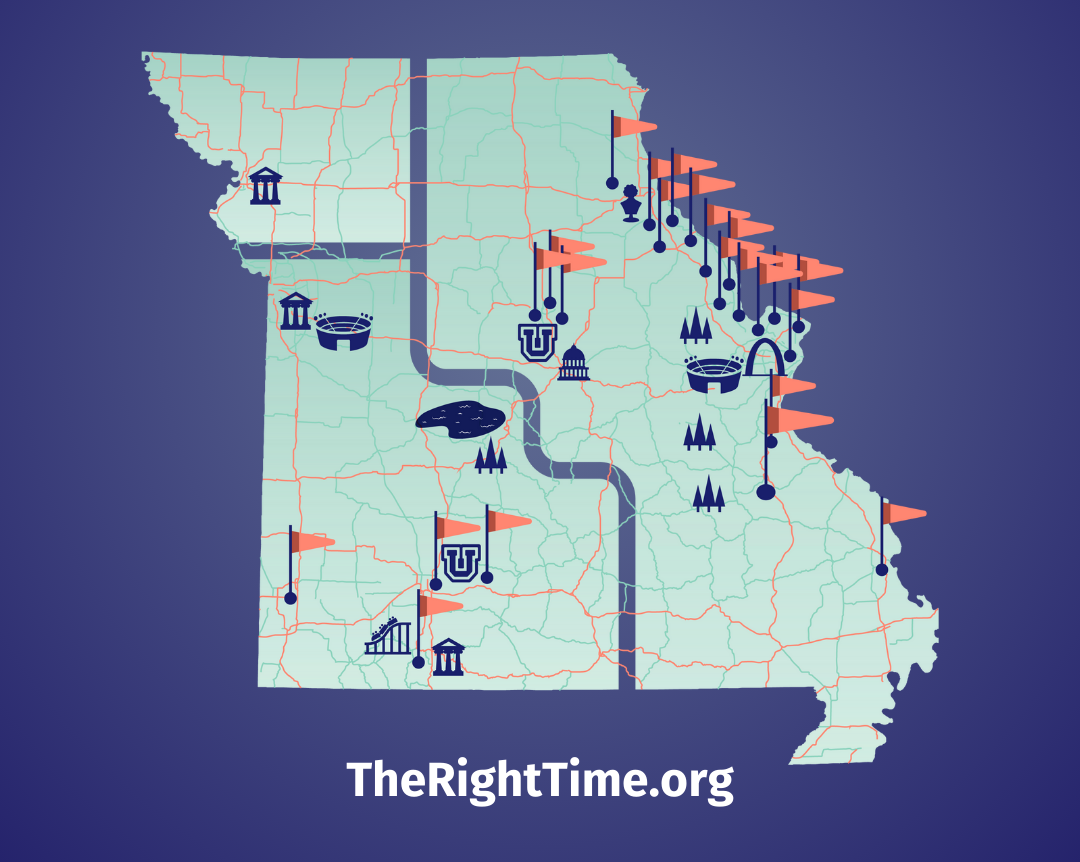
A positive HPV test can feel scary, but healthcare providers at your nearest The Right Time clinic can help.
As the new year begins, January marks Cervical Cancer Awareness Month. Here’s what you need to know, and what you can do in 2026, to protect your health.
HPV and Cervical Cancer: What’s the Connection?
HPV is an extremely common sexually transmitted infection. There are over 150 strains (types) of HPV, and most of them are considered “low-risk” infections that go away on their own. However, there are others that are considered “high-risk” and are associated with cervical, anal, and throat cancers. When these high-risk HPV infections don’t go away on their own, abnormal cervical cells can develop, and eventually, in rare cases, lead to cancer. Most cervical cancer is caused by Human Papilloma Virus (HPV).
Finding out you have HPV is common and not the same thing as having cancer. Most HPV strains do not have any symptoms, which is why regular check-ups with your provider for HPV screens and Pap smears are important. A positive HPV test can feel scary, but healthcare providers at your nearest The Right Time clinic can help explain what it means, what follow up looks like, and how to monitor things safely.
How Cervical Cancer Screening Works:
When precancerous changes (abnormal cells) are caught early through screening, treatment is much more effective. There are two options to screen for cervical cancer. Most of the time, to check for abnormal cells, a provider collects a sample from the cervix. This is done by performing a Pap smear. It’s a routine exam where a provider inserts a speculum into the vagina and uses a wand-like tool to collect cells from the cervix that are then sent to the lab for testing. A newer option for cervical cancer screening is HPV self-collection, where you collect your own vaginal sample using a swab.
Different organizations have different recommendations on when to start cervical cancer screening, which screening tests to use, and routine follow up intervals. But, for average risk patients, the US Preventative Services Task Force recommends screening starting at age 21, with Pap testing every 3 years until 29. And then from age 30-65, it’s recommended to get a Pap test with high-risk HPV testing every 5 years or Pap without HPV testing every 3 years. For people opting for HPV self-collection, the American Cancer Society recommends beginning screening at age 25 and getting screened every 3 years.
Prevention:
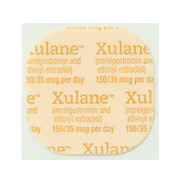
Beyond screening, vaccination is one of the most powerful tools to prevent high-risk HPV infections. The Gardasil vaccine is a series of two or three shots that protects against 9 strains of high-risk HPV viruses. While it’s best to start the HPV vaccine series early, before you have sex, it’s not too late to prevent HPV infections and decrease your risk of cancer by getting vaccinated now. You can still get the vaccine even if you know you have HPV or have had HPV in the past.
If it’s time for your recommended cervical cancer screening, make an appointment with your nearest The Right Time health center. This January, talk about HPV risk, screening, and vaccination with your partners.
Related Content


Article
What Does “Dual Protection” Birth Control Mean?It usually means using a condom along with another birth control method.

Article
Own Your Well-Being in 2026 with These 3 Sexual Health ResolutionsFirst: prioritize preventative sexual and reproductive health care.

Article
Birth Control & Your Period: What to ExpectBirth control often changes your period, and that’s normal and safe.