Which Birth Control Pill is Right for Me?

There are basically two different kinds of pills, the combination pill, and the mini-pill.
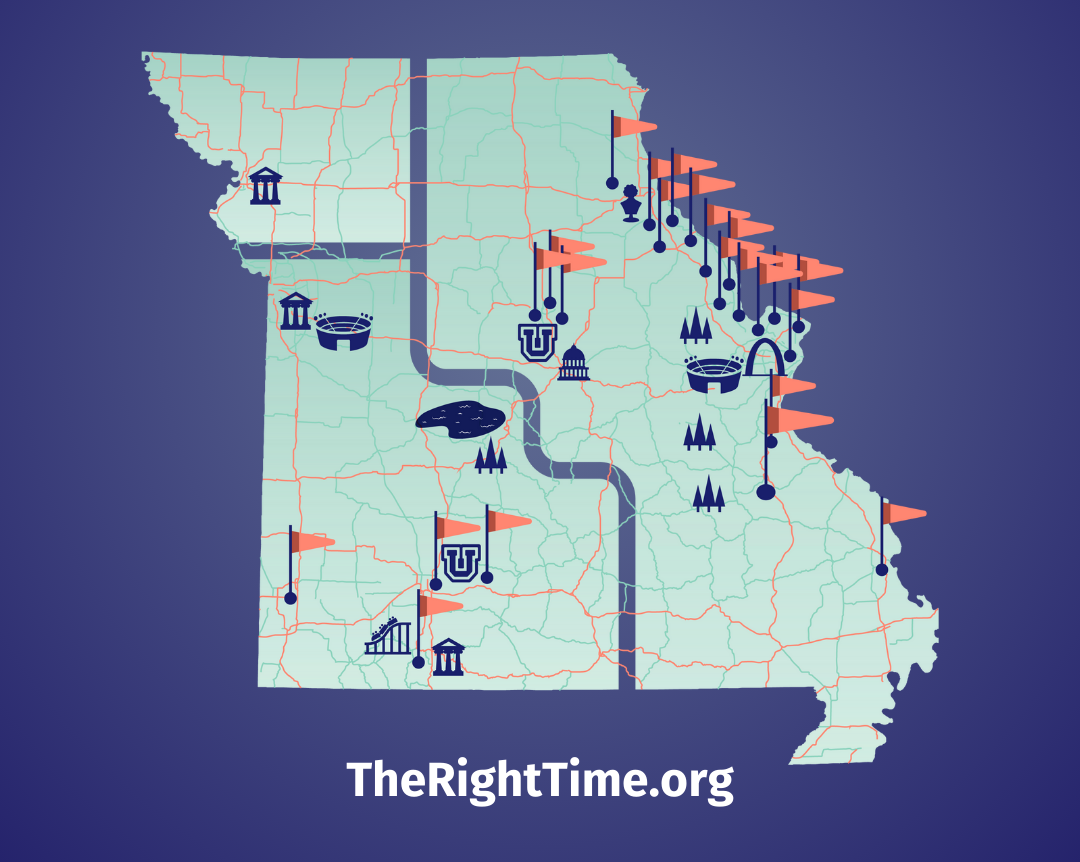
It’s always been more than just birth control. It helped spark the sexual revolution. It’s a feminist icon that’s been letting women live life on their own terms for 50+ years. If you’re thinking about using it, here’s everything you need to know to find the right one. For even more information or counseling, you can head over to your nearest The Right Time health center.
While an IUD or implant may make more sense if you don’t want to get pregnant for at least a year or two, the pill is a bit more flexible. Most types of birth control pills should be completely covered by health insurance, but if you don't have health insurance, you can get them for free or at a low cost from a The Right Time-affiliated provider.
Different kinds of pills and how they work
The pill is made of synthetic hormones like those that occur naturally in your body. There are basically two different kinds of pills, the combination pill, and the mini-pill.
Combination pills
Combination pills contain two types of hormones, estrogen, and progestin. They prevent pregnancy in three ways: by suppressing ovulation (meaning your eggs stay put in your ovaries); by thickening cervical mucus (making it harder for sperm to move); and by thinning the lining of the uterus (making it harder for an egg to attach there). This type of pill is more widely used than the mini-pill. (BTW, the patch and ring also contain both estrogen and progestin and have the same efficacy and safety profiles as combo pills.)
Combination pills vary by type of progestin and amount of estrogen. (They either have 35 or 20 micrograms of estrogen.) Different pills also have different amounts of hormone over the course of the month.
“Monophasic” pills have an even amount of hormone throughout the month.
Other pills have varied hormone doses through the month, most commonly three doses in “triphasic” pills. There's no evidence that triphasic pills have any benefit when compared to monophasic pills among large groups of women.
A note on brand names: In terms of efficacy or “good” side effects like better skin and periods, no brand of the pill has been shown to be more effective than any other, which means there’s typically no medical reason to use an expensive name-brand pill.
Combination pill names: Alesse, Apri, Aranelle, Aviane, Enpresse, Estrostep, Lessina, Levlen, Levlite, Levora, Loestrin, Mircette, Natazia, Nordette, Lo/Orval, Ortho-Novum, Ortho Tri-Cyclen, Yasmin and Yaz. (Not quite as clever as nail polish names, but they get the birth control job done.) Lybrel, Seasonique, and Seasonale (generic names: Jolessa or Qualsense) are combo pills that can minimize periods to just a few times a year or less.
Benefits: Combination pills are linked to less crampy, lighter, shorter periods. (That can also mean less chance of anemia.) These pills may also clear up acne. The combo pill reduces the risk of ovarian and endometrial cancer.
Combination pills might not be right for you if: you are sensitive to estrogen’s side effects like nausea or breast tenderness. To help with estrogen’s side effects, you can try lower-dose combination pills, which contain less estrogen, but they might cause more between-period bleeding (a.k.a. spotting).
You should not take the combination pill if: you have certain health conditions like high blood pressure or migraines with aura. The combination pill is also contraindicated (meaning risky to your health) if you smoke and are over 35. It’s important to know that if you have a contraindication, the amount of estrogen doesn’t matter—it’s not safe to use any method that contains estrogen at all. The bottom line is it’s always important to talk to a health care provider about your medical history before starting a new birth control method. One more thing: If you’ve given birth recently, you should avoid combination pills and other methods with estrogen.
Heads up: The combo pill might be advertised as highly effective, but in real life about one in 10 women become pregnant while using it. This can be for a range of reasons, from missing pills to changes in a woman’s metabolism. It can also be less effective against pregnancy if you use it while taking any of the following: the herbal supplement St. John’s Wort; HIV and seizure medicines; topamax/topiramate, which can be used to treat seizures or migraines; or the antibiotic rifampin, which is used to treat tuberculosis. (Other antibiotics are fine to take with the pill.) These medicines limit your body’s ability to adequately absorb the pill’s pregnancy-preventing hormones. If you take these meds, consider a birth control method that doesn’t contain estrogens, such as the mini-pill, an IUD, the shot, or the implant.
Inactive pills: There are typically four to seven inactive or placebo pills in each monthly pack. These are the pills that have no or a low dose of hormones. You take these to maintain your daily habit of taking your pill at about the same time each day.
Mini-pills
Mini-pills contain only progestin. They prevent pregnancy by thickening your cervical mucus and thinning the lining of the uterus. Some mini-pills suppress ovulation, but that’s not the main way they work. The mini-pill was developed for women who are sensitive to estrogen. It has the same failure rate as the combo pill—about one in 10.
Mini-pill names: Camila, Errin, Jolivette, and Micronor.
Benefits: The mini-pill is safe for people who are at risk of heart disease or strokes, or are heavy smokers. It’s also safe when you’re breastfeeding.
Inactive pills: Unlike the combo pill formulas, every mini-pill in your pack is active. Take one every single day, at about the same time each day.
Popular pill-related questions
Can I use the pill to have my period less often, or to skip a month once in a while?
Yes. If you have heavy, painful periods, or conditions that make your menstrual cycle suck—like migraines, endometriosis, or epilepsy—then skipping periods could be awesome.
Most combination pills contain 21 active pills and seven placebos, or 24 active pills and four placebos. You usually get your period when you’re taking the placebo-pills. To skip that month’s period, don’t take the placebos—just go straight on to the first active pill in the next month’s pack. Read more about skipping periods with the pill (or the ring) and talk to your provider if you’re interested in this option. Note: This only works for combo pills, not mini-pills!
Newer combination pill formulations have been developed that give you four or fewer periods a year. Instead of a 28-day pill pack, they typically come in packets of 84.
What other birth control methods contain estrogen?
Like the combination pill, the patch and the ring both contain estrogen and progestin. Progestin-only methods include the mini-pill, the shot, the implant, the Mirena and Skyla IUDs, and levonorgestrel-based emergency contraceptive (EC) pills.
Isn’t estrogen for women going through menopause?
It can be. Our bodies’ estrogen surges during puberty and declines during menopause, which typically occurs anywhere between ages 40 and 55.
Some women use estrogen pills, patches, or creams to relieve the hot flashes, vaginal dryness, or other not-so-fun symptoms of menopause. Progestin is also used in some hormone-replacement therapies to protect the lining of the uterus from developing cancer. Estrogen also helps your body process calcium. Females who lack estrogen—because they are menopausal, or don’t have periods because of intense athleticism or eating disorders—can be at risk of osteoporosis.
Is there a connection between the pill and cancer?
Recent studies show no difference for pill takers or non-pill takers. Other studies indicate the combo pill reduces the risk of ovarian and endometrial cancer, and maybe colon cancer too.
Everything in life comes with possible risks and benefits, including pregnancy—which researchers say poses many more health risks than does the use of hormonal birth control. Because so much depends on your body, the safest route is always to discuss your family history and any other concerns with your health care provider.
And when it comes to birth control information, always keep in mind that some organizations and individuals exaggerate or twist the possible links between hormonal birth control and disease because they want to scare women away from having sex outside of marriage.
The truth is, medical researchers have found that the pill can decrease your risk of some cancers. Again, you’ll have to weigh the benefits and risks to find out if the pill is right for you.
What about the pill and migraines?
Some people who experience migraines say the pill makes them better, others say just the opposite, and some say the pill makes no difference at all. Wish we had a definitive answer here, but your mileage may vary.
People under 35 who have migraines without aura generally do fine on any type of hormone-based birth control. Those who have migraines with aura, and any migraine sufferer over age 35 (with or without aura) should generally not use estrogen-containing methods due to increased risk of stroke.
If the combination pill or some mini-pills keep my eggs from being released, does this mean that I’ll remain fertile longer than I would off the pill? Say I take the pill from age 18 to 40; will all those eggs still need to come out one by one in the form of continued periods after I stop taking the pill?
Nope. Your eggs don’t “store up” in this fashion. They age and tend to dissolve and break down over the years. There’s no real difference between pill takers and people who never used hormonal birth control when it comes to how old you’ll be when menopause begins.
My friend loves her pill. Should I just go on that one too?
Maybe, but you still have to discuss it with your health care provider to find out for sure. Just because it works for your best friend doesn’t mean it’s the perfect pill for you and vice versa. Everybody is different, and you really have to try it to know if it’s right for you.
Updated July 2021
Related Content


Article
What Does “Dual Protection” Birth Control Mean?It usually means using a condom along with another birth control method.

Article
January is Cervical Cancer Awareness Month: What to Know About HPV and ScreeningA positive HPV test can feel scary, but healthcare providers at your nearest The Right Time clinic can help.

Article
Own Your Well-Being in 2026 with These 3 Sexual Health ResolutionsFirst: prioritize preventative sexual and reproductive health care.