My glamorous life with HPV

Everything you should know about HPV—from one of the 80% of women who will have it.
“Just want to give a shout-out to all my HPV ladies out there,” is a thing I posted recently in an online forum for young women. The comment was in response to a poll that asked, “Do you have any STDs?”
Whenever someone asks me (usually in a medical setting) if I have any STDs (a.k.a. STIs, for sexually transmitted infections), I always almost forget that I do. But then I remember: Oh yeah, I have HPV. Because who doesn’t? The CDC estimates that 80% of sexually active women will have it by the time they’re 50. HPV is so common that it feels like it doesn’t even count. But, it does.
People in their early 20s, a.k.a. people with great immune systems, are the most likely group to get HPV (which stands for human papillomavirus). This explains why 90% of people who get the virus will fight it off with nothing more than their immune system in less than two years time. I’m part of the other 10%—a very elite club who have a persistent HPV infection, because for whatever reason, our bodies can’t fight off the virus. I’ve had HPV for three (beautiful) years.
In that time, I’ve gotten to know HPV pretty well. It’s a glamorous life of pap smears, colposcopies, biopsies, cryotherapy, the legendary Loop Electrosurgical Excision Procedure (LEEP) and seeing your gynecologist so often that you have her personal cell phone number, and you guys text sometimes. Also, you send her Christmas cards, and you don’t even really send Christmas cards.
Anyway, in the three years I’ve been living with HPV, I’ve picked up a few things. Let’s start with the basics:
A-B-C H-P-V (The Basics)
Of the more than 150 strains of HPV, at least 40 can be passed through sexual contact. Some of these strains cause genital warts; some of them act stealth and present no symptoms at all. It’s just everyone’s luck that the stealthiest strains happen to be the ones that can do the most damage.
High-risk strains
The medical community knows that at least 13 stealthy, high-risk strains exist, and that the HPV-16 and HPV-18 strains are the suckiest. Together, those two strains contribute to the development of over 70% of HPV-related cancers.
Low-risk strains
A comparable number of HPV strains cause genital warts. In fact, the combined power of the HPV-6 and HPV-11 strains causes more than 90% of genital warts cases. Although these strains cause unbecoming things to grow on your genitalia, they’re low-risk because they don’t cause cancer.
Exposure and diagnosis
Even if you understand how common HPV is, getting a diagnosis probably won’t feel as shrug-worthy as it should. A lot of scary unknowns get thrown at you, and you’ll probably find yourself wanting to make sense of them. Sometimes this panicked sense-making leads you to blame someone.
You may want to blame the person who gave you HPV
Unless you’ve only had sexual contact with one person and that person absolutely, positively knew they had HPV and didn’t tell you, consider the following:
HPV’s incubation period—the time between when you are initially exposed and when it shows up in your system—can range between one month and years. If you’ve had more than one partner in the past few years, you might not be able to know for sure who passed it to you.
To make it more complicated, there’s no test to detect HPV in the throat and mouth, which mostly affects males. There isn’t an HPV test for guys to detect asymptomatic strains (the ones that don’t cause genital warts) either.
Oh, one more layer of complication: For the most part, the standard tests used to diagnose HPV in females (different from a Pap smear and pelvic exam) don’t call out specific strains of HPV. (However, there are several different HPV tests and certain strains can be detected, so if you test positive, ask your health care provider if you want more information.)*
Even with some serious investigative work and pattern-tracing, it’s pretty tricky to confidently solve this case. Let it go, detective.
You may want to blame yourself
When all the facts indicate that blaming whomever gave you HPV is pointless and/or impossible, you might move on to blaming yourself. Maybe you tell yourself you should have been more careful, refrained from sex, or had “safer” sex, somehow.
But, here’s the deal: Protecting yourself from HPV is no easy task. Even if you used a condom—even if you never had sex involving penetration, you can pass and contract HPV with skin-to-skin contact. I said it before and I’ll say it again: It’s so common—you don’t need an explanation to give to anyone, especially yourself.
Of course, that’s not to say you should blow off trying to protect yourself. You should do everything you can, such as a) use condoms, b) get tested regularly for STIs, c) get the HPV vaccine and d) all of the above.
Prevention and the HPV vaccine
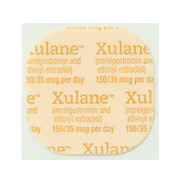
Two HPV vaccines are currently available across the U.S.: Gardasil and Cervarix. Both require you to get three shots over a period of six months, and both protect against HPV-16 and HPV-18 (the super evil strains). Gardasil also protects against the HPV-6 and HPV-11 strains (the ones notorious for causing genital warts).
It’s recommended that anyone between the ages of 11 and 26 get vaccinated, ideally getting the first shot around the age of 11 or 12. Unfortunately, lots of girls, and even more boys, aren’t getting all three shots.
Whether you have HPV or not, get the HPV vaccine
By the time the HPV vaccine had fully hit the market, I was 24 years old. It wasn’t easy to find, at least not back then. When I finally found it and got the first shot, I was 25 and still on my mom’s health insurance plan. When I turned 26 and aged out of her plan, I also aged out of the recommended age window for the vaccine.
Changing my insurance meant finding a new doctor. Finding a new doctor meant finding a doctor who could give me the vaccine… again. Time passed, as did the due date for my second dose. I had so many questions, and because the vaccine was still new, it was hard to find the answers.
Could I still get the second shot, or did I have to start the vaccine over? Would starting over even be an option at age 26? If you’ve already gotten one shot and you’re late getting the second one, you don’t need to start the vaccine over—you just get the next dose as soon as you can. It’s believed (but not 100% proven) that the vaccine works even if you miss a dose or receive doses later than recommended.
Would being 26 prevent me from getting the second shot? The age that matters is the age when you start the vaccine and get the first shot. So while the recommended ages to get the vaccine stop at 26, there’s nothing in place to stop someone 26 or older from getting the vaccine if they really want it.
Do I really even need to get all three shots? Is there any chance just getting one could work? More research is needed, but so far evidence suggests that the vaccine works best if you get all three shots.
Shortly after I received my second dose (late), I was diagnosed with HPV. At first I assumed my diagnosis rendered the need for the third shot obsolete, but, my doctor told me I should still get it. Because the HPV test only reports a positive result and doesn’t identify what strain causes the positive result, the vaccine could still be useful in protecting me from strains that I (hopefully) hadn’t contracted.
A note for those older than 26 who haven’t been vaccinated
As a newly diagnosed 26-year-old getting her final vaccine shot post-HPV-diagnosis, it dawned on me that I didn’t understand why 26 was the recommended age cutoff—obviously it was possible to get HPV at age 26.
So, I looked into it. To sum it up, the medical community assumes that by a certain age (26), you’ve already had sex and probably been exposed to HPV. They also assume that your immune system has already fought it off, whether you’re aware of it or not. All of this matters because the vaccine can only protect you from an HPV strain if you’ve never had it before—not if you had it and your body got rid of it.
So if you’re 26 or older, it might be worth it for you to get the vaccine if you fit the following description:
You’ve had very few sexual partners (like one or two)—and your sexual partners had very few sexual partners, and so on.
You’re currently not in a committed, long-term relationship, and/or think you’ll have a new sexual partner in the future.
If this sounds like you, talk to your health care provider about your sexual history to suss out if getting the vaccine might be a wise choice. It never hurts to ask.
Looking forward
When it comes to navigating HPV, keep in mind we’ve only taken one step on a very long journey. New treatments will come out, and new statistics and complications will sneak their way into the spotlight. Keep an eye on some of the following developments:
Scientists don’t know for sure how long the vaccine works—they only know it stays effective for at least six years.
In December 2014, the FDA approved a new version of Gardasil, “Gardasil 9”, that protects against five additional high-risk HPV strains. It should become more widely available with time—get it if you can!
HPV is associated with more than 11,000 cases of cervical cancer (in women) and more than 12,000 cases of oropharyngeal cancer (in men and women, with the majority being men) a year. The latter cancer statistic is a rapidly rising trend, especially for guys.
Finally, remember that even though HPV seems to be everywhere, it doesn’t mean the battle to disband the elite HPV-forever clubs is hopeless. Prevention is the key. So, to all the ladies and gents out there—whether you’ve got HPV or not—do all you can to protect yourself and inspire others to do the same. The more the ones you love protect themselves, the more you yourself are protected, too.
*Editor’s Note: A previous version of this article incorrectly implied that there are no tests to detect any specific strains of HPV. It has been edited to reflect the fact that certain high-risk strains can be individually identified.
Related Content


Article
What Does “Dual Protection” Birth Control Mean?It usually means using a condom along with another birth control method.

Article
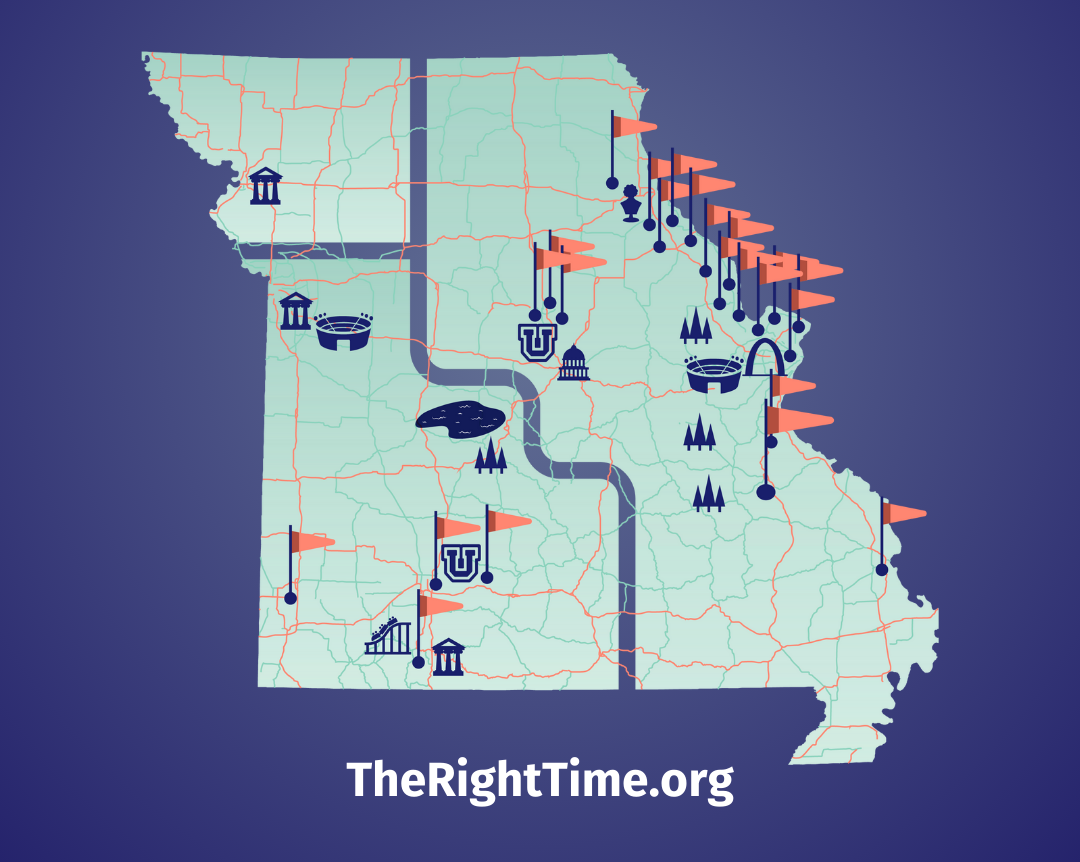
January is Cervical Cancer Awareness Month: What to Know About HPV and ScreeningA positive HPV test can feel scary, but healthcare providers at your nearest The Right Time clinic can help.

Article
Own Your Well-Being in 2026 with These 3 Sexual Health ResolutionsFirst: prioritize preventative sexual and reproductive health care.