Which Medications Can Mess with Birth Control?
Certain meds do interfere with birth control—not most antibiotics, though.
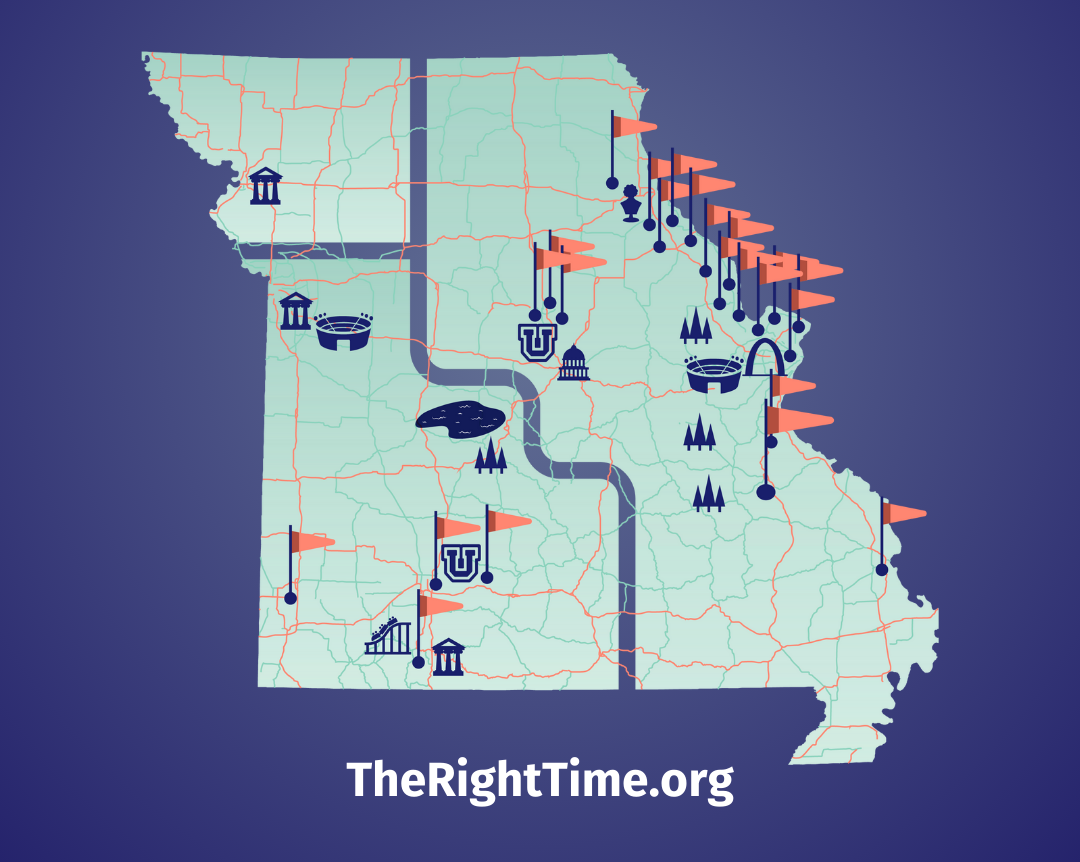
Many women using birth control with hormones—including the pill, the patch, and the ring—have heard that antibiotics can make these methods less effective. Thankfully, that’s not true for most antibiotics. But there are medicines that can interfere with some kinds of birth control. Let’s talk details, why these meds mess with birth control, and what alternatives women taking these meds have. For more personal guidance, talk to a provider at your nearest The Right Time health center. They stock all methods of contraception and offer free or low-cost contraception to those who need it.
Antibiotics
Most antibiotics do not make the pill, patch, or ring less effective—that includes antibiotics commonly prescribed for acne (doxycycline, tetracycline), a sore throat (ampicillin), a urinary tract infection (ciprofloxacin), or a vaginal infection (metronidazole). Lots of women who use the pill have also used these antibiotics, so scientists have heaps of data to prove that these antibiotics do not impact birth control.
So how did this rumor get started? It started with stories—“OMG, my best friend’s cousin’s neighbor was taking an antibiotic and she got pregnant”—and spread from there. If you’re taking antibiotics for diarrhea or nausea, being so ill may make it harder to absorb the pill, or harder to remember to take it. If you take the pill and have severe vomiting or diarrhea, check with your health care provider to see if you need to alter your dose. When in doubt, use a condom for backup.
There is one important exception: For women being treated for the lung infection tuberculosis, the hardcore antibiotic commonly prescribed (rifampin or rifabutin) can interfere with the birth control pill. We have good evidence that rifampin messes with the pill and may also affect the patch and the ring. Since Rifampin therapy for tuberculosis generally lasts 6-9 months, a different contraceptive choice might make sense for you. If you are taking rifampin, or any of the rifamycin antibiotics (including rifapentine, rifalazil and rifaximin), talk to your provider about your birth control options. If you decide to stay on the pill, patch, or ring while taking this type of antibiotic, use a backup method like condoms every time you have sex.
Mood stabilizer & epilepsy medicines
Women taking some medicines to treat bipolar disorder or epileptic seizures have a double reason to choose their birth control carefully:
1) Many of the medicines used to treat epilepsy and bipolar disorder—Barbituates, Carbamazepine, Oxcarbazepine, Phenytoin, Primidone, Topiramate, Felbamate, and Lamotrigine when taken alone—make the pill, patch, ring, and mini-pill less effective, increasing the chance of an accidental pregnancy.
2) There’s some evidence that these methods of birth control change the effectiveness of those particular medicines, too. That increases the chance of having a seizure, or a manic or depressive episode. If you have epilepsy or bipolar disorder, it’s really important to talk with your provider about what birth control method is best for you—there are still good options!
Medicines for HIV
Some medicines used to treat HIV (antiretroviral drugs) make the pill less effective. Examples of these drugs include Nevirapine and Nelfinavir- and Ritonavir-boosted protease inhibitors (like Darunavir, Fosamprenavir, Lopinavir, Tipranavir). There are antiretroviral drugs that do not mess with the pill, including Tenofovir. If you take an HIV medicine, talk with your health care provider about the risks and benefits of your birth control options.
St. John’s Wort
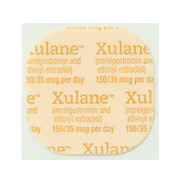
Saint John’s Wort is an herbal remedy that some people take for depression, anxiety or insomnia. Taking St. John’s Wort pills or extract reduces the concentration of both hormones (estrogen and progestin) in the pill by about 15%. For women taking the pill—especially a low-dose pill (20-35 micrograms of estrogen)—this changes the dose enough to make breakthrough bleeding more likely, but we don’t know exactly how this affects the risk of pregnancy. If you take St. John’s Wort and prefer to avoid taking risks with your birth control, consider using a method other than the pill, patch, or ring or use condoms to back them up.
How do these meds mess with birth control?
For the science geeks among us, here’s how this works: it’s all about metabolism, the process by which our bodies use and clear medicines. Just like with food, the body has an intricate and multi-step process for breaking down medicines, using them, and then clearing them from the body.
One of the key players for medicines is an enzyme (a special kind of protein that helps get work done) called the P450 system. The P450 system helps process both of the hormones in the pill, the patch, and the ring—estrogen and progestin. Some medicines speed up or slow down this enzyme system. If the system is revved up, it will go to work breaking down and removing the hormones faster than normal, resulting in lower levels of the hormones to get the job done. It can result in such low levels of hormone that the pill, patch, or ring don’t work.
What if I take a medication that messes with hormonal birth control?
There are many highly effective types of birth control that are not affected by these medications, including all IUDs, the implant, and the shot. Barrier methods like condoms are also effective regardless of what medication you’re taking.
In general, it’s good to remember that medicines can have powerful interactions with each other—and hormonal birth control is just another type of medicine. If a new medicine is prescribed for you, make sure to tell your health care provider about all of the medicines, herbal and vitamin supplements you regularly take.
Updated June 2019
Related Content


Provider Perspective
The Common Cold of the Sexually Active World: HPVLet’s talk HPV—causes, treatments, and prevention.
Provider Perspective
Skip the Pelvic, Please!What to expect when it’s time to visit your lady doctor. (It may just be a conversation.)

Provider Perspective
Does Being Overweight Affect Your Birth Control?When it comes to birth control and weight, not all methods are created equal...