5 Vasectomy Myths, Busted

Getting the snip gets a bad rap—but if you’re done with kids or never want any, don’t let rumors stop you from learning more.
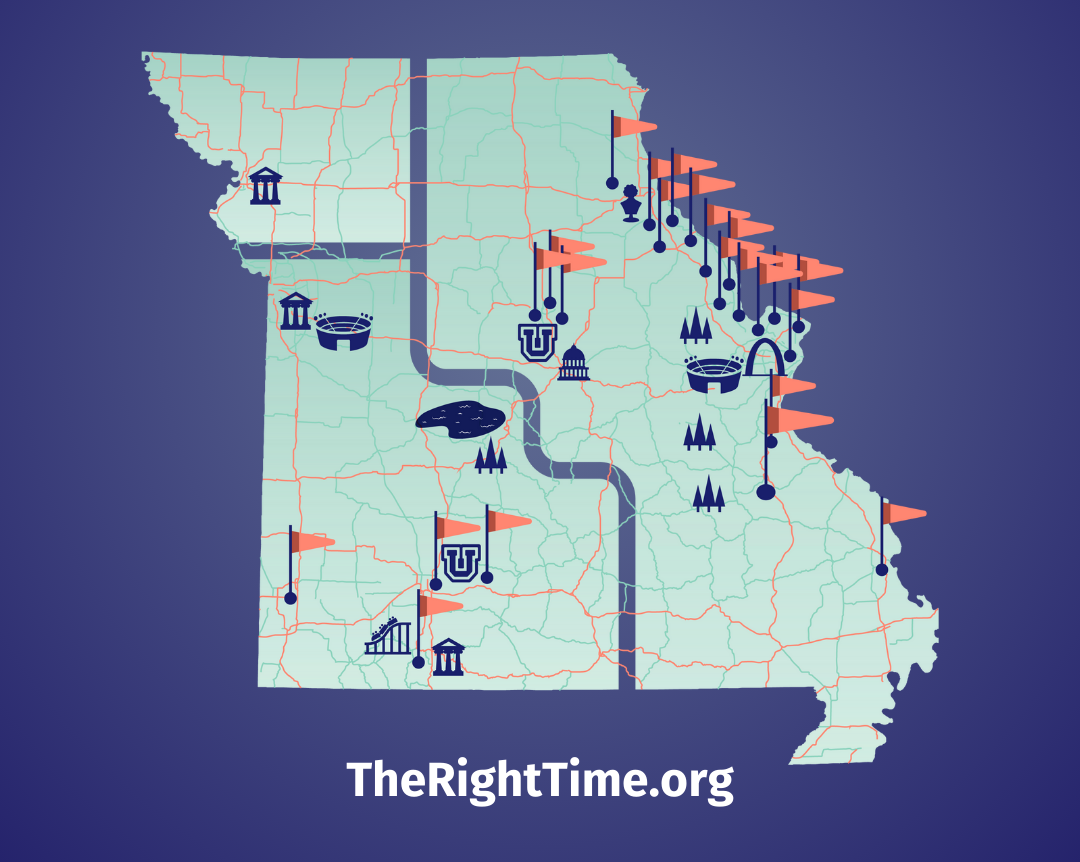
Vasectomy, a.k.a. male sterilization is often thought of—or not thought of—as the “other” form of sterilization. Female sterilization is much more common, even though vasectomy is just as effective, safer, and costs less. Let’s take a closer look at this misunderstood method of birth control, and if you're interested in learning more, talk to a provider at your nearest The Right Time health center. They stock all methods of contraception and offer free or low-cost contraception to those who need it.
Myth 1: Getting a vasectomy is painful—maybe even dangerous.
We hear you—you’re wary of any operation involving the family jewels. Fortunately, vasectomy is very safe and is done as an outpatient procedure. The procedure itself takes about 10-20 minutes, though many providers will also require a separate counseling visit (20-30 minutes). Vasectomy is always performed with anesthesia, which can be given by a standard needle, mini-needle, or jet-spray. The anesthesia is usually the most uncomfortable part—on average, 2 out of 10 on a pain scale. The vasectomy procedure itself is rated 0.5 out of 10 on average on the same scale. After getting a vasectomy, you should rest for 1-2 days, avoid heavy lifting for a week, and wear tight underwear and use cooling packs (or frozen peas) to minimize pain and swelling. Most people who get a vasectomy only need over the counter pain medications (e.g., Tylenol, ibuprofen) and can return to regular activity, including sex, after a week.
Myth 2: I won’t be able to get an erection or have an orgasm.
A vasectomy works by blocking the tube where the sperm travels. The tube starts at the epididymis where sperm is produced, passes the prostate and the seminal vesicle where sperm meets up with other fluids that make up semen, then comes out through the urethra. A vasectomy blocks the part of this tube near the testicles, so the penis is not affected in any way. Studies show that men who have a vasectomy report no change in their libido or their ability to have an erection or an orgasm.
Myth 3: Vasectomy causes prostate cancer.
This is a myth that emerged in the 1990s and reemerged in 2014 based on studies that seemed to show an association between vasectomy and prostate cancer. Both times, the studies faced criticism for problems with their design and methodology. The flawed studies sparked larger, better-designed studies, and these studies showed no connection between vasectomy and prostate cancer. The American Urological Association reviewed all the data and weighed in to say that vasectomy does NOT cause prostate cancer.
Myth 4: Vasectomy is the same as castration.
Castration is the removal of the testicles (balls). As described in myth 2, vasectomy only affects the tube the sperm travels through, so your testicles remain intact and totally unharmed.
Myth 5: My sperm will build up and my balls will explode.
After a vasectomy, your body continues to produce sperm. But where does the sperm go when the tube has been blocked? The sperm doesn’t build up—it’s just reabsorbed by the body as it’s produced. Some people may temporarily form a sperm granuloma due to an inflammatory reaction during the absorption process, but this typically resolves in 2-4 weeks and can be treated with an anti-inflammatory painkiller like ibuprofen.
A vasectomy is a great form of permanent birth control, so if you’re done having kids or know you don’t want any, don’t let myths and misinformation stop you from considering it. Want to learn more? Visit a provider at a The Right Time health center to talk about your options.
Updated June 2019
Related Content


Provider Perspective
The Common Cold of the Sexually Active World: HPVLet’s talk HPV—causes, treatments, and prevention.
Provider Perspective
Skip the Pelvic, Please!What to expect when it’s time to visit your lady doctor. (It may just be a conversation.)

Provider Perspective
Does Being Overweight Affect Your Birth Control?When it comes to birth control and weight, not all methods are created equal...