5 Things Your Provider Wishes You Knew About Birth Control

No, it doesn't affect your fertility.
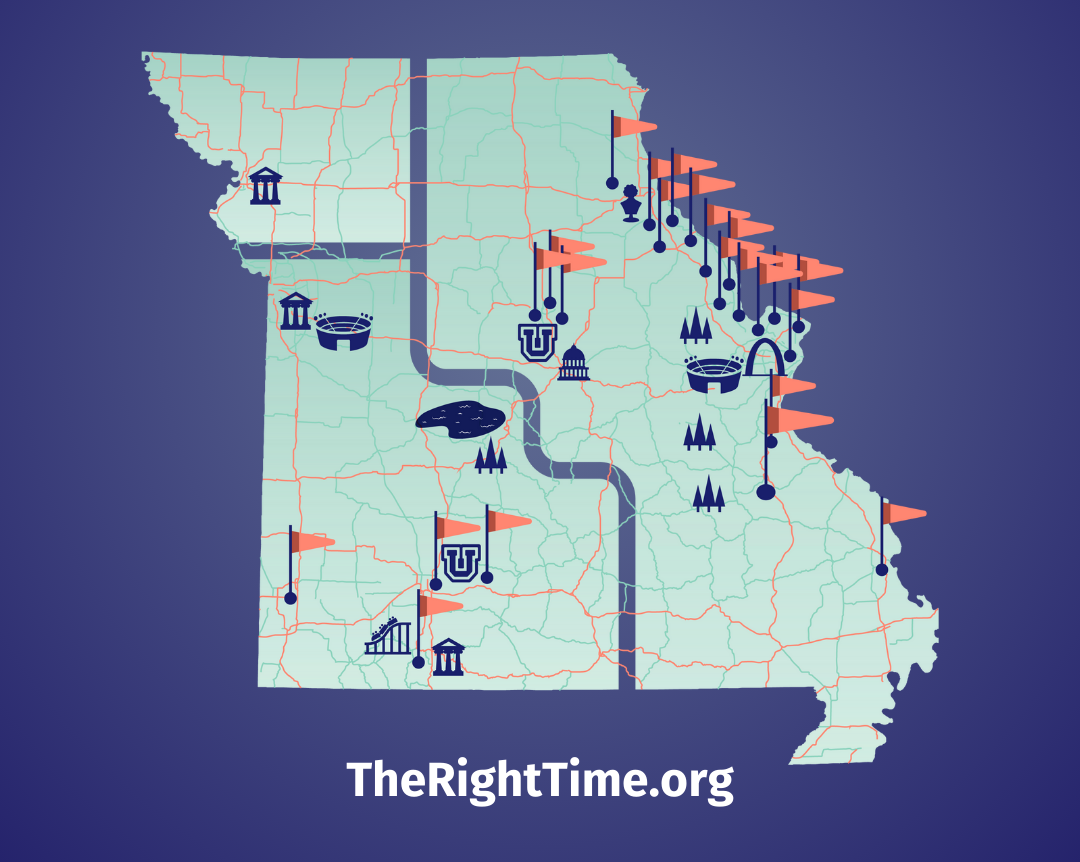
In my practice, I have heard from a lot of people about their worries and concerns about birth control. There are some really common misconceptions out there, and I understand how it can be hard to separate what’s true from what’s not. I would like to clear some of them up here, in the interest of helping to empower patients everywhere to choose a method of birth control that’s right for them. If you have additional questions—or simply want to get a method of birth control—call or head to your nearest The Right Time health center.
1. Using birth control now doesn’t affect your chances of getting pregnant in the future.
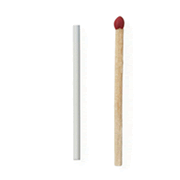
The truth is that there is no birth control that changes your chances of getting pregnant in the future (other than permanent methods like having your tubes tied or a vasectomy). If you use a method that has to be used every time you have sex to prevent pregnancy, like condoms, internal condoms, or the diaphragm, you can get pregnant anytime you have sex and don’t use your method. If you are using the pill, the patch, the ring, the hormonal IUD, or the implant, you can get pregnant within a day to a few weeks after stopping your method. If you are using the shot, the hormones stay in your body for at least 13-15 weeks after your last shot, and it’s possible to get pregnant as soon as one day after the shot wears off. For some people, the hormones in the shot can stick around for up to nine months and decrease your chance of getting pregnant during that time. Talk to your provider to see if this may be the case for you. If you are using the non-hormonal IUD, you can get pregnant as soon as it is removed, even the same day.
You may have heard someone say they couldn’t get pregnant after being on birth control, but difficulty getting pregnant is caused by things that most people don’t think about until they go off birth control and try to get pregnant. Things like how old you are, a history of pelvic inflammatory disease (which can cause scarring that blocks the fallopian tubes and makes it harder for eggs and sperm to meet), or endometriosis can all affect your chances of getting pregnant but being on birth control doesn’t change that. After you stop using any method of birth control, your chance of getting pregnant goes back to what is normal for you.
2. Birth control is a healthy choice.
All the FDA-approved birth control methods have gone through extensive research showing they are safe to use and effective at preventing pregnancy. Some even have other benefits, like making your periods shorter, giving you periods with less cramping, and improving acne. For some people, like those with PCOS (polycystic ovarian syndrome is a hormonal disorder), using birth control to regulate their periods now can actually increase their chances of getting pregnant in the future.
Even though birth control is safe, not every method is a good fit for everyone. Some people, like those with high blood pressure or a history of the type of blood clots that can cause a stroke, shouldn’t use methods that have estrogen, like the patch, the ring, or some types of the pill, since estrogen can increase the risk of having a blood clot. And some people just don’t want to use hormones at all. The good news is that there are hormonal methods without estrogen for people who need them, like the hormonal IUD, the shot, the implant, and the mini-pill. There are also methods without any hormones at all, like the non-hormonal IUD and condoms. You might have to try a few to find the right one for you, but there is a method out there to fit your life!
3. There may be an adjustment period.
Changes to your period, breast tenderness, nausea, and other side effects can happen when you start any new method. These changes don’t mean that there is something wrong. Methods that only have progestin, like the shot, the implant, the hormonal IUD, and the mini-pill are likely to change your periods. How much your bleeding will change is hard to predict. With progestin-only methods it would be normal (and safe), for you to have no bleeding, bleeding that comes and goes, or even bleeding every day. So, if it’s important to you to have a regular, predictable period, these methods might not be a good fit for you. Instead try the pill, the patch, the ring, or any non-hormonal method, like condoms, internal condoms, or the non-hormonal IUD.
For other birth control methods with hormones, like the pill, the patch, and the ring, it would also be safe and normal to have changes to your period. While some people don’t notice a change to their periods, you could have bleeding between periods, lighter periods, or no periods at all. Some people even use these methods to safely skip their periods altogether.
Most of the time symptoms like nausea and irregular bleeding get better after a few months. At any time, if you are not happy with your method, it’s always okay to switch. Sometimes it takes trying a few methods to figure out which one works for you and your life.
4. You don’t need to take a break from birth control.
In fact, there is no medical need to take a break from birth control to “clean out your system” or for any other reason.
The truth is, the hormones in birth control are out of your system so quickly that if you don’t want to get pregnant immediately after you stop taking birth control, think about starting another method right away to stay protected. If you have sex while you are not using birth control, or if you have a whoops moment and don’t want to get pregnant, consider using emergency contraception to prevent pregnancy.
5. We aren’t here to judge.
The best method for you today might be totally different than what is best for your sister, your friend, your provider, or even what was perfect for you last year (or last month). Thinking about what is most important to you in a method, like having regular periods, being able to keep it private, or having one that also protects you from STIs, can help you find a method. But it’s also okay (and very common) to try different methods until you find one that works for you and your life.
Updated December 2019
Related Content


Provider Perspective
The Common Cold of the Sexually Active World: HPVLet’s talk HPV—causes, treatments, and prevention.
Provider Perspective
Skip the Pelvic, Please!What to expect when it’s time to visit your lady doctor. (It may just be a conversation.)

Provider Perspective
Does Being Overweight Affect Your Birth Control?When it comes to birth control and weight, not all methods are created equal...