5 Myths about the Emergency Contraceptive Pill, Busted

When it comes to post-sex pregnancy prevention, don't believe the rumors.
Emergency contraception pills (ECPs) are the subject of more rumors and misunderstandings than any celebrity I can name—despite the fact that the medical community has been studying them for over 50 years. Part of the confusion is due to outdated information included in package labeling, and part is due to political interference with science.
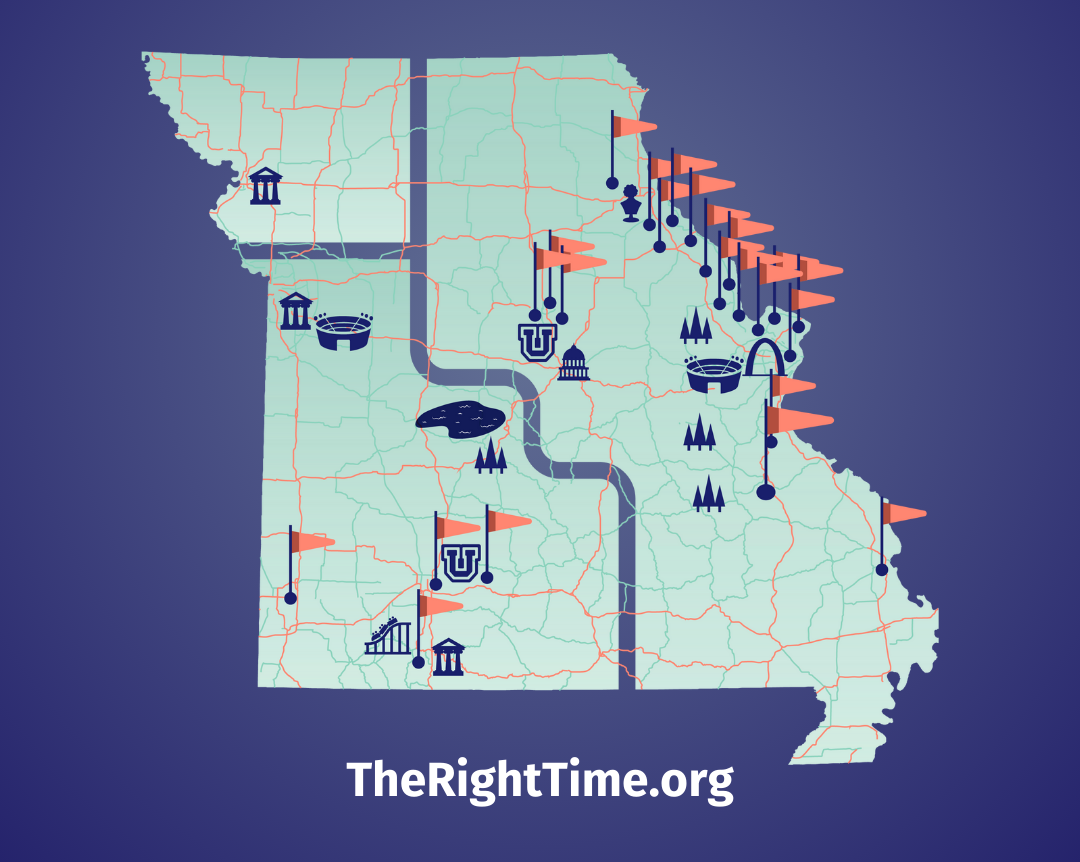
If the condom broke, you forgot a pill, or things went further than you planned, having a Plan B—pun intended—can make a big difference. So if you ever had, have, or might have sex, it’s important to separate the fact from the fiction where ECPs are concerned. Here's the truth behind these 5 common myths about emergency contraception, and for more immediate help, contact a provider at your nearest The Right Time health center. Remember, they stock all methods of contraception and offer free or low-cost contraception to those who need it.
Myth 1: There’s only one ECP option—and it’s hard to get.
There are more than two dozen types of ECPs in the U.S. The most common is the levonorgestrel-only pill—the best-known brand of it is Plan B One-Step and generic versions include Next Choice One Dose, My Way, and Take Action. Plan B One-Step and generic levonorgestrel-only ECPs are now available in pharmacies, in stores, and online without a prescription or age restrictions. Most health centers accept walk-in patients who need emergency contraception (EC) in a hurry.
A newer ECP called Ella contains ulipristal acetate and requires a prescription regardless of age. You can consult with a doctor and get a prescription for Ella online. Side effects are low with either method, but some women have nausea, abdominal cramps, or changes in their next period. BTW, it’s also good to know that a study found that levonorgestrel-based pills may be less effective for women who weigh more than 165 lbs—and Ella may be less effective for women who weigh more than 195 lbs. Paragard is the only EC option that we know is equally effective regardless of weight.
There’s also the Yuzpe method, where plain old birth control pills taken in higher amounts can be used as EC. This table shows the needed amounts for different types of pills. This method may be convenient, especially if birth control pills are already on hand, but it’s associated with more nausea and vomiting and is less effective than other options.
Getting ECPs as quickly as possible after unprotected sex is important since their effectiveness decreases over time. The idea is to take them immediately after sex, but they can help prevent a pregnancy when taken up to five days after.
Myth 2: ECPs cause abortion.
Little-known fact: After sex, sperm hang around in the fallopian tubes for days waiting for an egg to appear. If an egg doesn’t show up, the sperm eventually gives up. That’s why ECPs only work for up to 5 days after sex, and why it’s important to take them as soon as you can.
Some people confuse ECPs with medication abortion pills, but they are not the same thing. (At all.) Levonorgestrel, the progestin hormone in most ECPs, has no effect on an established pregnancy. All ECPs prevent pregnancy by delaying ovulation, so the egg and sperm never meet up. Studies show that ECPs are not effective if a woman has already ovulated.
Myth 3: I partied last night, so taking ECPs now is dangerous.
Alcohol, tobacco, and other drugs don’t change the effectiveness of ECPs. Partying may affect how likely you are to hook up, but there’s no reason for it to affect your decision to take EC the next day. In general, the benefits of taking ECPs far outweigh the risks—especially since not taking it can mean dealing with the risks that come with pregnancy. It makes sense if you think about it like this:
EC is a one-time dose of a higher level of a hormone your body makes naturally.
Pregnancy is a nine-month dose of those same hormones at even higher levels.
Myth 4: If I take ECPs today, I’m covered if we have unprotected sex again tomorrow.
ECPs are only good to protect against one act of unprotected sex. They work by blocking ovulation, but only for a few days, so if you take them and have unprotected sex again afterward, you’re significantly increasing your risk of pregnancy. If you have unprotected sex again within a few days of taking the pills, there will be more sperm waiting in the fallopian tubes when the egg is eventually released.
Myth 5: ECPs will mess up your fertility if you take them too many times.
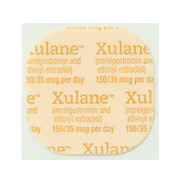
There is zero evidence that taking ECPs multiple times affects future fertility. ECPs prevent about 7 out of 8 pregnancies that would otherwise occur, meaning they’re less effective than other types of birth control like the pill, patch, and ring. ECPs are way less effective than the IUD or implant. Also, depending on your health insurance, it may be expensive to take them repeatedly.
If you find you’re taking ECPs regularly, it’s probably more affordable—not to mention more effective—to talk to a The Right Time health care provider about which non-emergency method of birth control could be right for you. But if you ever have an emergency situation, don’t believe the rumors—ECPs are a safe and effective second chance to prevent accidental pregnancy.
Updated June 2019
Related Content


Provider Perspective
The Common Cold of the Sexually Active World: HPVLet’s talk HPV—causes, treatments, and prevention.
Provider Perspective
Skip the Pelvic, Please!What to expect when it’s time to visit your lady doctor. (It may just be a conversation.)

Provider Perspective
Does Being Overweight Affect Your Birth Control?When it comes to birth control and weight, not all methods are created equal...